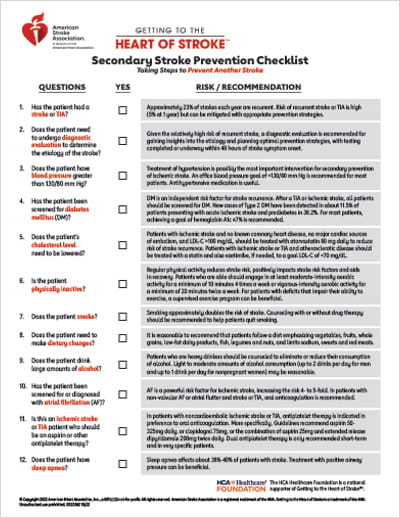
Secondary Stroke Prevention Checklist
Getting to the Heart of Stroke™ | Taking Steps to Prevent Another Stroke
Download the Secondary Stroke Prevention Checklist (PDF)
| QUESTIONS | YES | RISK / RECOMMENDATION |
| 1. Has the patient had a stroke? | The risk of a recurrent stroke is 6% at 1 year, 16% at 5 years, and 25% at 10 years post stroke. | |
| 2. Has the patient experienced a TIA? | Approximately 12% of all strokes are preceded by a TIA. | |
| 3. Has the underlying cause of the stroke been identified? | If the etiology of the stroke has not been determined, consider collaborating with colleagues to further evaluate the cause. | |
| 4. Is this an ischemic stroke patient who should be on an aspirin regimen? | Guidelines recommend that Aspirin (50–325 mg/d) monotherapy or the combination of aspirin 25 mg and extended-release dipyridamole 200 mg twice daily is indicated as initial therapy after TIA or ischemic stroke for prevention of future stroke. | |
| 5. Does the patient have uncontrolled high blood pressure? | Treatment of hypertension is possibly the most important intervention for secondary prevention of ischemic stroke. Target blood pressure for secondary stroke prevention should be <130/80 mm Hg. | |
| 6. Does the patient have diabetes mellitus (DM)? | DM is an independent risk factor for stroke recurrence. After a TIA or ischemic stroke, all patients should be screened for DM. | |
| 7. Does the patient’s cholesterol level need to be lowered? | "Statin therapy with intensive lipid-lowering effects is recommended to reduce the risk of another ASCVD event. The first goal is to achieve a ≥50% reduction in LDL-C levels, but if LDL-C levels remains ≥70 mg/dL on maximally tolerated statin therapy, adding ezetimibe may be reasonable." therapy, adding ezetimibe may be reasonable. | |
| 8. Is the patient physically inactive? | Physical activity improves stroke risk factors, may reduce stroke risk itself, and aid recovery. For patients who are capable of engaging in regular physical activity, at least 3 to 4 sessions per week of 40 minutes of moderate- to vigorous-intensity aerobic physical exercise are reasonable to reduce stroke risk factors. | |
| 9. Does the patient smoke, or are they exposed to second-hand smoke? | Current smokers have a 2 to 4 times increased risk of stroke compared with nonsmokers. Talk to your patient about programs, nicotine replacements and other medications that can help them quit. | |
| 10. Does the patient need to make | It is reasonable to do a nutritional assessment of your patient. Patients should be counseled to follow a diet emphasizes vegetables, fruits, whole grains, low-fat dairy products, fish legumes and nuts, and limits sodium, sweets and red meats. | |
| 11. Does the patient drink large amounts of alcohol? | Patient who are heavy drinkers should be counseled to eliminate or reduce their consumption of alcohol. Light to moderate amounts of alcohol consumption (up to 2 drinks per day for men and up to 1 drink per day for nonpregnant women) may be reasonable. | |
| 12. Does the patient have sleep apnea? | A sleep study might be considered for patients with an ischemic stroke or TIA. Treatment with CPAP might be considered for patients with ischemic stroke or TIA and sleep apnea. | |
| 13. Has the patient been diagnosed with atrial fibrillation (AFib)? | AFib is a powerful risk factor for ischemic stroke, increasing the risk of stroke by five times. It is reasonable to consider a combination of oral anticoagulation therapy and antiplatelet therapy in patients that have CAD, ACS or stent placement. |
© Copyright 2022 American Heart Association, Inc., a 501(c)(3) not-for-profit. All rights reserved. American Stroke Association is a registered trademark of the AHA. Getting to the Heart of Stroke is a trademark of the AHA. Unauthorized use prohibited.
The HCA Healthcare Foundation is a national supporter of Getting to the Heart of Stroke™.