Atherosclerosis and Stroke
Often referred to as hardening of the arteries, atherosclerosis can lead to heart disease and stroke. It’s a slow, complex disease that typically starts in childhood and progresses with age.
How it progresses
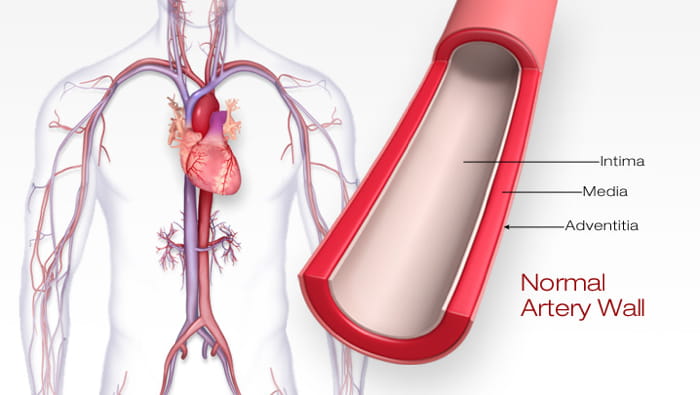
Atherosclerosis usually affects large and medium-sized arteries. It starts when the inner lining of an artery (the endothelium) is damaged. This damage may occur from physical stress, such as high blood pressure. High blood cholesterol or high blood sugar and inflammation driven by the immune system may also cause artery damage.
Fats, cholesterol, platelets, cellular debris and calcium gather in the walls of damaged arteries, stimulating the creation and accumulation of other types of cells. Fat builds up within and around these cells, and connective tissue forms. This buildup is called plaque.
The plaque thickens the artery wall, narrowing the vessel. Narrowing decreases blood flow, reducing oxygen supply to the part of the body the artery serves.
Stroke and atherosclerosis
Atherosclerosis can lead to two types of ischemic stroke.
Atherothrombotic stroke is the most common. Sometimes, plaque in a blood vessel breaks. Blood clots can form where the plaque ruptures. These clots can become large, reducing or blocking blood flow. When blood flow to the brain is blocked, a stroke occurs.
Sometimes a blood clot or other particle breaks away from the rupture site. The bloodstream carries that wandering clot or particle (called an embolus). When it lodges, blocking blood flow in an artery leading to or in the brain, it results in an embolic stroke. However, most embolic strokes are from blood clots that form due to atrial fibrillation and then enter the bloodstream.
View a detailed animation of atherosclerosis.
Risk factors for atherosclerosis
Males and people with a family history of premature cardiovascular disease have an increased risk of atherosclerosis. Other risk factors include:
- High blood pressure: Damages the lining of blood vessels, making them susceptible to atherosclerosis
- High blood cholesterol and triglycerides
- Diabetes mellitus
- Cigarette smoking and exposure to tobacco smoke (the chemicals in cigarettes can cause damage to blood vessels, speeding up the process of plaque buildup)
- Unhealthy eating habits
- Older age: In men, the risk increases after age 45; in women the risk increases after the age 55.
- Family history
- Physical inactivity




